Traumatic Brain Injury
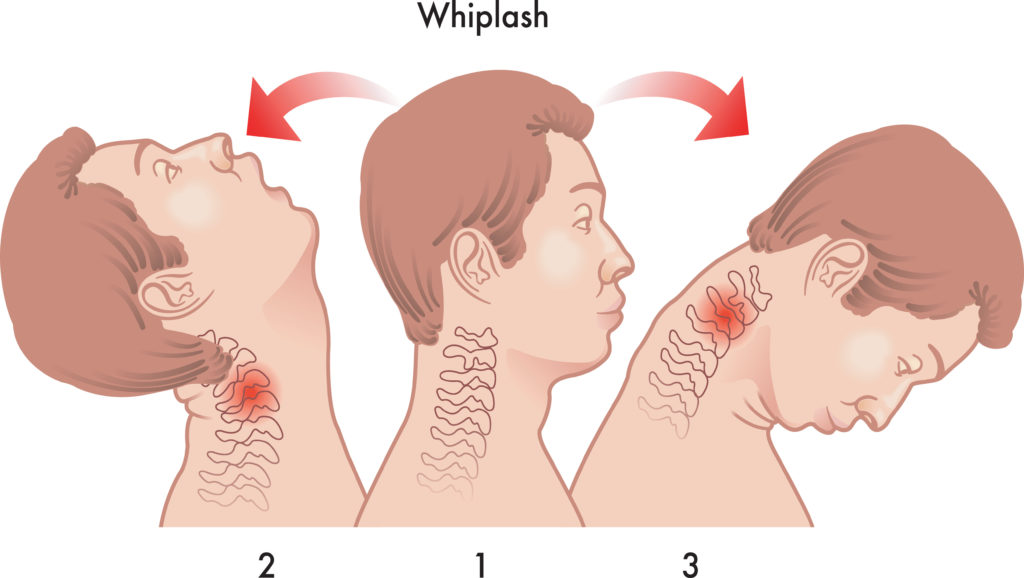
A traumatic brain injury or TBI is a disruption in the normal functioning of the brain. This can be caused due to a sudden bump or blow to the head as in the case of a car accident. It can also occur when an object pierces the skull and enters the brain tissue or due to the head hitting an object all of a sudden. This can be observed as alterations in the functioning of the brain. For example, the person may feel disoriented, become slow thinking or have difficulty in concentrating. It can also lead to a loss of consciousness or decreased consciousness, loss of memory about events that occurred before or after the memory loss, change in speech, loss of vision and focal neurological deficits like muscle weakness.
Depending on the extent to which the brain is damaged, the symptoms can vary from mild to moderate and severe. A brief change in the mental state or consciousness may be observed if the symptoms are mild. However, if the symptoms are severe, it may lead to long periods of unconsciousness, coma or death.
According to the data from the Centers for Disease Control and Prevention (CDC), in 2014 out of 2.87 million TBI cases around 837,000 were children. In the US alone about 13.5 million people live with disability caused by TBI. Every year 288,000 people are hospitalized due to TBI. These figures are at least 20 times more than those for spinal cord injuries.
TBI among children
Traumatic brain injury figures among young children 14 and below are equally alarming. They account for around 837,000 emergency room visits, 23,000 hospitalizations and 2,529 deaths each year. Around 80,000 to 90,000 persons suffer long-term or lifelong disabilities related to TBI. The numbers are higher for males (78.8%) than for females (21.2%) although overall men outnumber women in TBI related accidents.
Sports and recreational activities
At least 21% of all TBI cases among children and adolescents in the US can be attributed to sports and recreational activities. TBI statistics show that the highest TBI numbers, 2232 per 100,000 are found among older adults aged 75 and above, while among children ages 0 to 4 it is 1591 per 100,000 and youth between 15 and 24 years old it is 1081 per 100,000.
Most TBI deaths are due to car accidents and crashes, suicides and falls. Around 34% of all traumatic deaths occur due to head injuries. According to data from Centers for Disease Control and Prevention (CDC), the leading cause of non-fatal TBI in the US is due to falls (35%), car accident injuries (17%) and blows to the head or sports injuries (17%).
Signs and symptoms
Symptoms of TBI vary depending on the seriousness of the head injury. It can cause a headache, vomiting, confusion, lethargy, paralysis, loss of consciousness or even coma. Symptoms include changes in vision such as dilated pupils, blurred vision, inability to tolerate bright light, loss of eye movement and blindness. Other symptoms include dizziness and balance concerns, breathing problems, slow pulse, slow breathing rate with increase blood pressure or cerebrospinal fluid appearing from the nose and ears. TBI can also cause ringing in the ears or hearing, inappropriate emotional responses, cognitive difficulties, speech difficulties like slurred speech, inability to articulate or understand words, difficulty in swallowing, loss of bowel or bladder control, numbness or tingling in the body and droopy eyelid or facial weakness. If you observe any of the above symptoms after a car accident and suspect TBI, rush the person to a hospital immediately or call for an ambulance.
Are you looking for physiotherapy or a chiropractor? Book an assessment today at EAST (Scarborough) 3630 Lawrence Ave E, Scarborough, ON M1G 1P6 or 200 Marycroft Ave UNIT 6, Woodbridge, ON L4L 5X9, Canada.
Types of Injuries
Traumatic brain injuries can cause mass lesions leading to contusions and hematomas and increase pressure inside the brain. Let us look at the different types of injuries that can occur as a result of TBI.
Hematoma
A hematoma is a blood clot in the brain or on its surface. It can happen anywhere in the brain. When there is blood collection between the dura mater (protective cover of the brain) and inside the skull it is called an epidural hematoma. When the blood collection happens between the dura mater and the arachnoid layer (the surface of the brain), it is called a subdural hematoma.
Contusion
Bruising of the brain’s tissue is called a cerebral contusion. Cerebral contusions are similar to bruises in other parts of the body, when looked at through a microscope. The injured part of the brain gets swollen and mixed with blood that has come out from the veins, arteries and capillaries. Generally contusions are found at the base of the front part of the brain although they can occur anywhere.
Intracerebral hemorrhage
Intracerebral hemorrhage or ICH refers to the bleeding that happens within the brain’s tissue. It can be related to other brain injuries such as contusions. Depending on the size and location of the hemorrhage, it may be possible to remove it surgically.
Subarachnoid hemorrhage
Subarachnoid hemorrhage or SAH refers to the bleeding that happens in the subarachnoid space. This usually occurs after TBI and looks like diffuse blood is spread over the surface of the brain. Although most cases of SAH associated with head trauma are mild, severe traumatic SAH may cause hydrocephalus.
Diffuse Injuries
TBIs can cause diffuse brain injury with or without associated mass lesion. Diffuse brain injury refers to the microscopic changes that are scattered throughout the brain but do not appear on CT scans.
Diffuse Axonal Injury
Axons are long extensions of nerve cells inside the brain that communicate with each other. Axonal injury is impaired function and gradual loss of axons. If several axons are impaired or hurt, the nerve cells may lose their ability to communicate with each other and to integrate their function. Such an impairment of axons can result in severe disabilities in the person.
Ischemia
Ischemia, also a diffuse injury, refers to an insufficiently low levels. This is very critical because the brain has just gone through a traumatic injury and is sensitive to reduced blood flow. Blood pressure changes can have a negative impact immediately after the head injury.
Skull Fractures
TBIs can occur along with simple cracks or linear fractures in the skull. If the force is strong enough to damage and fracture the skull, it can also damage the brain underneath it. Skull fractures in the base of the skull are problematic. They can damage the nerves, arteries or other structures. If such a fracture extends into the sinuses, it can cause leakage of the cerebrospinal fluid (CSF) from the ears or nose of the person. Even if a part of the bone presses into the brain, it can cause depressed skull fractures.
Testing and Diagnosis
People with TBI, whether moderate or severe, need urgent medical attention. Since it is not possible to reverse the initial damage to the brain due to the trauma, doctors try to stabilize the person affected with TBI and then try to prevent further injury. They first check the cardiac and pulmonary functioning of the patient and then move on to a quick examination of the whole body. This is followed by a complete neurological examination using the Glasgow Coma Scale (GCS). They also assess the ability of the pupils to contract in bright light. A wide or dilated pupil on only one side indicates presence of large mass lesions.
Doctors may also test brainstem reflexes including gag and corneal blink.
Radiological Tests
Radiological tests include computed tomography scan (CT or CAT scan), X-rays, and MRIs. The gold standard for radiological assessment of a TBI patient is a computed tomography scan. A CT scan is useful in detecting the presence of blood and fractures, the most crucial lesions in medical trauma cases. For patients with mild neurological dysfunction, X-rays of the skull are suggested. However, CT scanning is more accurate and available in most testing centers. For severe head injuries, magnetic resonance imaging or MRI is not recommended as it takes longer than a CT scan. Further, it is very difficult to transport a seriously injured person from the emergency room to a MRI scanner. After the patient’s condition stabilizes, it may be useful to do an MRI as it can show the presence of lesions that were not detected by the CT scan.
Information like this may be more useful to determine prognosis rather than treatment.
Surgery
Most accident victims and people with moderate or severe head injuries are taken to the operating room from the emergency rooms for surgery. The aim is to remove the large hematoma or contusion that is compressing the brain or increasing the pressure in the skull. Post-surgery they are kept under observation in the ICU.
Other patients with head injuries are normally taken from the emergency room to the ICU. These patients are not operated upon for days after the injury because the hematomas and contusions may enlarge for few hours/days after the head injury. When a patient’s neurological examination worsens or their intracranial pressure (ICP) increases, delayed hematomas may be revealed. Usually a routine follow-up CT scan indicates whether a small lesion has changed in size and that the hematoma has enlarged. It is best to remove the lesion before it enlarges and results in neurological damage.
Before the surgery is undertaken, the hair from the affected part of the head needs to be shaved off. Once the scalp is cut, the removed bone is extracted in a single piece and replaced after surgery. Incision of the dura mater is done carefully to examine the underlying brain. The hematoma or contusion is then removed by the neurosurgeon who ensures that there is no bleeding. Then the dura is closed, the bone is replaced and the scalp is closed again. Some neurosurgeons may not replace the bone if the brain is swollen. They may wait till the swelling decreases. Also the surgeon may choose to place an ICP monitor or other type of monitor. The patient is then taken back into the ICU for additional care and observation.
Non-Surgical Treatments
Currently, medication to prevent nerve damage or promote nerve healing after TBI is not available. The aim of the ICU is to prevent any secondary injury to the brain. The initial trauma to the brain is referred to as the ‘primary insult’, and the ‘secondary insult’ refers to any subsequent development to neurological injury. An injured brain is particularly sensitive and vulnerable to a decrease in blood pressure. This can be achieved through normal or slightly elevated blood pressure levels. Neurological damage can become worse if there is an increase in ICP, increase in body temperature, decrease in blood oxygenation, increase in blood glucose, and other similar disturbances. The main role of ICU management here is to prevent secondary insults in patients with head injuries.