Intermediate Exam
Examination Date: 2014-06-11
Chief Complaint
1. Bilateral Lower Back
Frequent bilateral lower back pain. Patient has been having lower back pain for the past four years. His medical doctor has suggested possible surgery. He regards this symptom as moderate and rated the pain as a 7 on a scale of 0 to 10 with 10 being the worst. The pain is reported as aching and dull, experienced most often during the night, after light physical activities and after moderate physical activities and is stated as radiating into the left buttock, left calf, right buttock, right calf and right hip. The pain is lessened by resting while bending and lifting aggravates the condition.
Capabilities of Daily Living
The patient states that capabilities of daily living have been affected in the following areas:
Due to pain, I am not able to lift heavy objects. However, light to medium weight objects are manageable. I experience MODERATE pain, which causes a significant limitation on my physical performance of activities. Pain is FREQUENT, and occurs between 50% and 75% of my awake time.
Physical Examination
Physical examination revealed an individual who was alert, cooperative and orientated.
The patient’s gait appeared normal. Minor’s sign was negative.
Sex: Male
Age: 60
Height: 175 cm
Weight: 72 kg
BMI: 23.5
BP: 101/66
Pulse: 71/bpm
Complexion: Normal
Size: Normal
Grip strength: Normal bilaterally.
Posture
There is no indication of a head tilt in the patient’s posture. He had a forward head carriage. The patient has rounded shoulders. There was a high right ilium. Observation and inspection of the thoracic spine revealed a normal spine. Profile view of the lumbar spine revealed normal curvature. Romberg’s test was negative. Adam’s sign was negative. Left heel walk: WNL. Right heel walk: WNL. Left toe walk: WNL. Right toe walk: WNL. Trendelenberg test on the left was negative. Trendelenberg test on the right was negative.
Ranges of Motion
Lumbar Spine
Motion Degree Normal Pain Level
Flexion: 19 60 Mild
Extension: 14 25 Moderate
Lateral Right: 15 25 Mild
Lateral Left: 12 25 Mild
Lumbar Spine Evaluation
Lumbar spine evaluation provided the following results:
Evaluation of the lumbar spinal region reveals tender areas in the lumbar region on both sides (grade 2) and erector spinae on both sides (grade 2). Palpation of the spine indicated discomfort and pain in the spinous process at: L4, L5 and S1 (grade 2). Evaluation of the lumbar spinal areas indicates that trigger points are present in the erector spinae bilaterally (moderate) and quadratus lumborum bilaterally (moderate). Straight leg raise was positive on the left (70 deg). The patient also reported experiencing radiating pain during the test. Straight leg raise was positive on the right. The patient also reported experiencing radiating pain during the test. Kemps was positive on the left. Kemps was positive on the right. Kemps test was positive for possible facet and meniscoid entrapment. Straight leg raiser test caused pain at 35 to 70 degrees for possible nerve root or disc involvement. This test was followed by Maximal SLR with internal rotation, adduction, foot dorsiflexion, neck flexion and patient bearing down to further pinpoint the lesion. Slump Test in a sited position was also performed to concur with space occupying lesion such as a disc herniation or a bulge. Milgram’s (double leg raiser) was also caused radicular pain due to increase of intrathecal pressure. Belt test made no difference during flexion with or without supporting the pelvis. Pain was also felt at hamstrings indicating tightness.
Diagnosis
Spinal Stenosis.
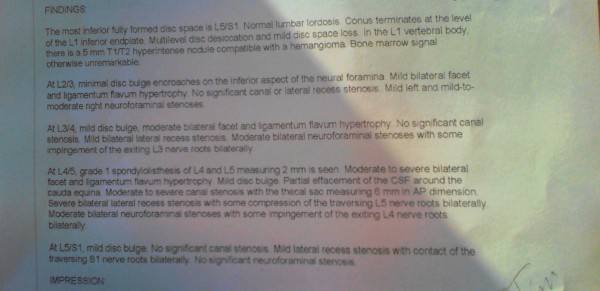
Consistent with MRI (22/2/2014) suggesting L4/5 grade 1 spondylolisthesis, facet liagamentum flavum hypertrophy, mild disc bulge, partial effacement of CFS around cauda equina, moderate to severe canal stenosis with the thecal sac measuring 6 mm in AP dimension. Severe bilateral recess stenosis with some compression of the transversing L5 nerve root bilaterally. Moderate bilateral neuroforaminal stenosis with some impingement of the existing L4 nerve roots bilaterally.
Management Plan
Short Term Goals would be for patient to report 50% pain reduction and 50% increase in ROM within 2 weeks. Functionally patient should also be able to perform half of his ADL’s within these 2 weeks easier. Long Term Goals would be for patient to report over 80% pain reduction and demonstrate over 80% increase in ROM within 4 to 6 weeks. Functionally patient should also be able to perform most of his ADL’s within this period. Patient is also to be discharged with a home exercise program when the above goals have been achieved and he is over 80-90% impairment free.
Chiropractic Spinal Decompression Therapy 3x per week/duration of 1 month
Today’s Treatments
Today’s treatment consisted of Chiropractic Spinal Decompression (Supine,6,60 lbs,-10deg and 20min NP) in the lumbar region.
Prognosis
The prognosis for the patient’s recovery is considered fair.
SOAP Notes – Detail
2014-06-27
Subjective Complaint
Mr. XXXXXXX was checked for his responsiveness to the treatment plan. Mr. XXXXXXX stated that his symptoms have gotten better since the last visit. Patient states that he is transferring, standing and walking, easier than before.
Objective
Tenderness was found in the lumbar region. Trigger points where noted in the lumbar area. Patient is able to transfer and stand, easier than before.
Lumbar Spine Evaluation
Lumbar spine evaluation provided the following results:
Assessment
The patient’s symptoms appear to be improved since the last visit.
Plan
Continue with therapies as directed. Mr. XXXXXXX should continue with the current treatment plan.
Today’s Treatment
Today’s treatment consisted of Chiropractic Spinal Decompression (Supine,2, 80 lbs,-10deg and 20min NP) in the lumbar region.
Notes:
Here is the initial exam and a follow up 6th visit. This particular patient has moderate so severe spinal stenosis at L4-L5 level. He is actually awaiting surgery. Although spinal decompression therapy is not a replacement for surgery but since the line-up to get on the surgical table is long we decided to treat this patient. To our own surprise he started feeling better after 2 sessions.
DOC settings of protocol #6 at 60 lbs with maximum flexion supine at -10 degrees was chosen. After couple sessions protocol #2 for longer pulls at the same angle and time with increase to 80 lbs was chosen.
Also Read
| Case Study: Acute Lumbar Radiculopathy (2) | Case Study: Chronic Lumbar Spinal Stenosis (3) | Case Study: Chronic Lower Back Pain | Case Study: Subacute Lower Back Pain |
| Case Study: Lumbar Spinal Stenosis | Case Study: Antalgic Posture | Case Study: L5-S1 Disc Prolapse | Low Back Osteoarthritis |
| Low Back Pain | Case Fruits: Acute Lower Back Pain |